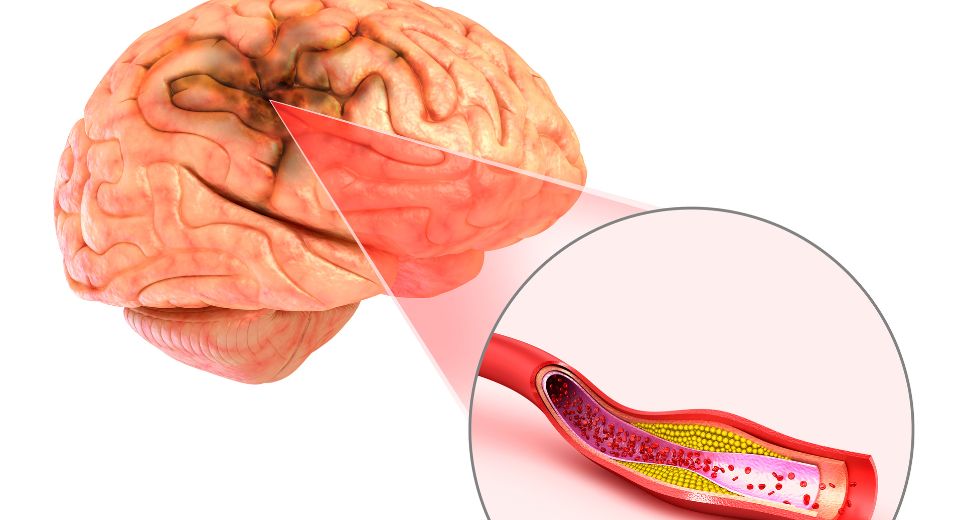
Ischemic Stroke: Causes, Risk Factors, Treatment, and Prevention
Ischemic stroke, a critical cerebrovascular event, is a condition in which the blood supply to a part of the brain is severely reduced or blocked.

Respiratory Syncytial Virus (RSV) in Children
Respiratory Syncytial Virus (RSV) is a respiratory virus with a large range of symptoms. It can affect all ages but usually acts like a common

Trick or Treat: A Parent’s Guide to Halloween Safety for Kids and Teens
Halloween is a time for fun and spooky surprises, but it’s also crucial to ensure that everyone, from the littlest pumpkin to the most wicked
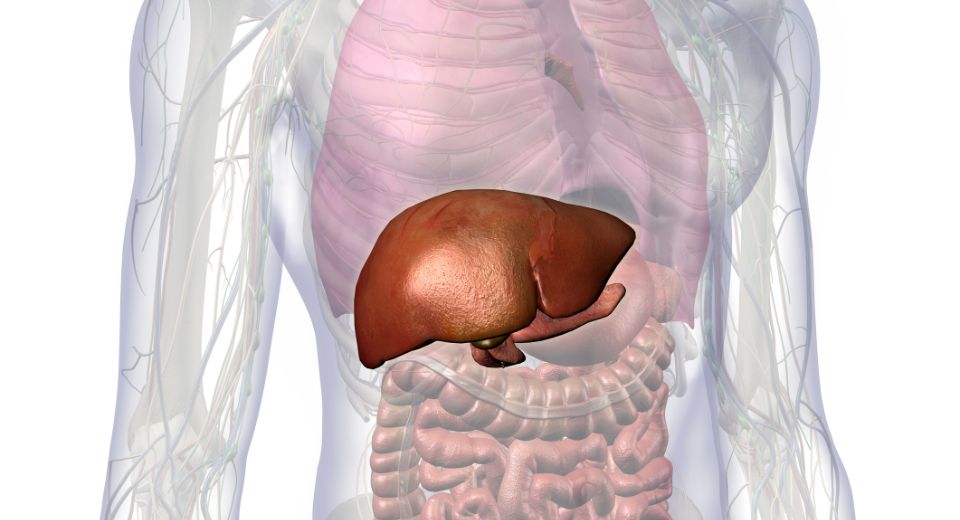
The Function and Purpose of the Liver
The liver, a remarkable organ in the human body, plays a pivotal role in maintaining our overall health and well-being. It is a vital part

Celiac Disease Awareness
Author: Nathan Kiskila, MD Celiac disease awareness day is every year on September 13th. About 83% of Americans who have celiac disease are undiagnosed or

Jet Lag
Author: Alyssa Sota, Manager We have all experienced the feeling of not being “in sync” when we arrive at our destination after crossing time zones

Kids and the Stomach Flu
Author: CHOC Pediatricians Gastroenteritis, also known as the stomach flu, is inflammation in the digestive tract, including the stomach and the small and large intestines.
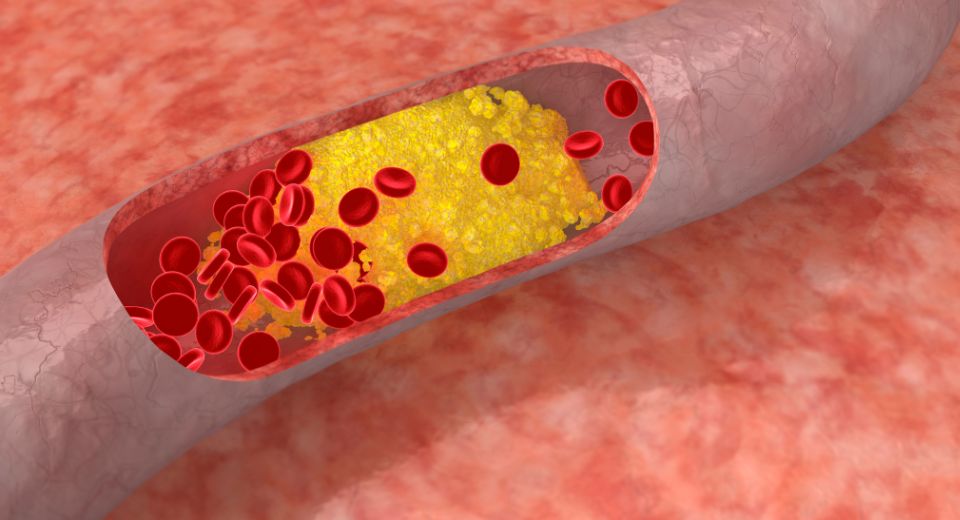
Ways to Lower Your Cholesterol
Author: Samuel Gerson, MD September is National Cholesterol Awareness Month. So, what is cholesterol and what are some of the ways to lower or maintain
Sepsis and Septic Shock
Author: Ryan Pham, PA-C September recognizes ‘World Sepsis Day’ every year on September 13th. Sepsis is a life-threatening condition when bacteria infect your bloodstream. It
