“BioPsychoSocial” is a hip buzzword in worker’s comp circles, but what does it really mean for employers, and how can the BioPsychoSocial model of healthcare potentially speed the recovery of an injured employee?
As a foremost expectation, health professionals treat the human body—the biological and physiological needs of the patient. Upon first meeting a physician, it is anticipated that there will be a thorough physical examination, taking vitals and testing reflexes, discussing health history and illnesses, as well as genetic and family history of disease.
Only in recent decades has the traditional biomedical model of medicine been challenged to include the psychological and social elements. The BioPsychoSocial model of health and illness as proposed by George Engel implies that:
“behaviours, thoughts and feelings may influence a physical state. He disputed the long-held assumption that only the biological factors of health and disease are worthy of study and practice. He argued that psychological and social factors influence biological
functioning and play a role in health and illness also.”(BMJ.com January 2015).
Biological & Psychological Assessment
In the treat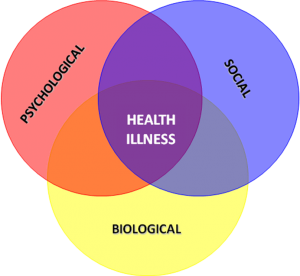
How a Social System Impacts Health
An injured employees’ social support system can also impact their ability to recover, and physicians can encourage patients to reach out to others for help. Having empathetic family members that provide compassion and support encourages overall wellness, and loved ones can help patients cope emotionally and physically. Friends and family can also reinforce the positive results achieved by following through with physical therapy exercises, either in a clinical environment, or at home, leading to faster healing.
According to a recent survey, claims adjusters rank
“psychosocial issues as the number one barrier to successful claim outcomes, according to Rising Medical Solutions’ 2016 Workers’ Compensation Benchmarking Study. A new white paper, co-authored by study program director Rachel Fikes and industry journalist Peter Rousmaniere, shows how claims advocacy principles…are taming the effects of psychosocial issues and coaching injured workers to recovery and claim resolution. Their short report – How to Overcome Psychosocial Roadblocks: Claims Advocacy’s Biggest Opportunity – examines key best practices, skill sets, and training approaches organizations are using to screen for, intervene in, and effectively address psychosocial factors. Rooted in advocacy, these strategies treat the injured worker…to proactively resolve non-medical barriers to timely recovery”
(WorkCompWire.com March 2017).
In conclusion, the BioPsychoSocial model of medicine attempts to treat not just the injury, but the whole person, with an approach that is mindfulness and holistic—speeding the recovery of the patient on both a physical and psychological level, and leading to overall wellness.

Favorite Platform

New Content




